Lauren Siegel is a Melbourne-based mum of two with a unique and inspiring fertility journey featuring IVF along with PGD (Pre-implantation Genetic Diagnosis). We were lucky enough to have Lauren share her story in Melbourne and we would love to share it with you all.
……………………………………………………..
Given the weight of recent events in Israel and across the globe, it has undoubtedly been a challenging and emotionally heavy time for all of us.
The past few weeks have been particularly tough to focus on preparing for this talk.
On October 7th, when AJFN asked me to share my story, it was a big fat yes! But since October 7th, the heaviness, the distraction, the PR war, and the rabbit hole of social media have all been very consuming. So, delving into a hard time in my life with a heavy heart was a challenge. I am going to do my best not to get too emotional. Please bear with me.
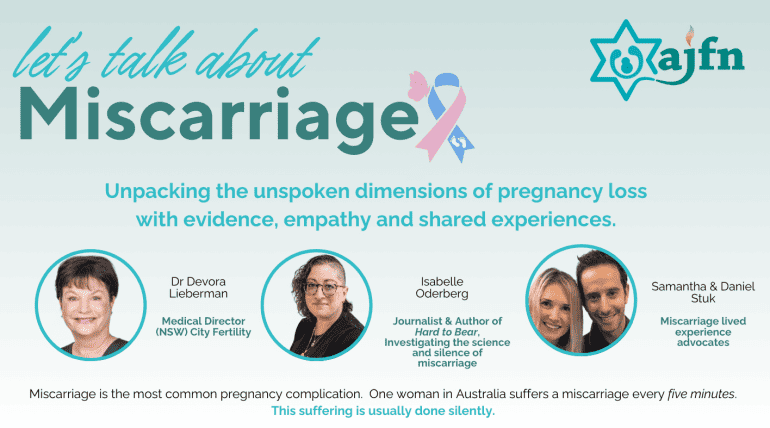
Firstly, what an amazing organisation AJFN is, it is an important initiative to support women and families going through something others might take for granted.
I am proud to stand here and share my story, my history on why we chose IVF, my struggles with my mental health during the process, the impact it had on my relationships, and the financial burden it put on our growing family. Welcome to my therapy session. You might want to grab some tissues. I have never done this before.
I am going to start with a happier sentiment…
I AM A MUM! Blessed with two beautiful girls, Taylor is 8 and Billie is 5. If you’re familiar with raising girls, you might understand when I say they think they are 15 & 16. It’s tough. And, of course, I’m equally blessed with a wonderful husband—well, most of the time! Jordan.
My story began when I was nine years old; back in 1994, my family immigrated from South Africa to Australia. Medical assessments are required to enter the country —X-rays, blood work, and scans. We did it all and gained entry into this incredible country.
Little did we know, my middle brother Ryan was living with a genetic heart condition.
It wasn’t until 2008, 14 years later, that tragedy struck. My brother Ryan, only 25 at the time, experienced the first symptoms of his heart condition, a sudden, fatal heart attack while celebrating his best friend’s bux party.
His passing led us, a mostly traditional Jewish family, to seek solace in the Jewish way of death and mourning. Something that brought a lot of comfort during a really hard time. The process after his untimely death was emotionally taxing. The coroner required an autopsy to release his body for burial—a traumatic but necessary step given the circumstances. A young fit 25-year-old dying in a public place.
Many Rabbis came to visit us in our home to give their advice. It was only Rabbi Genende’s counsel that resonated with us the most: He said, “If one future life can be saved from Ryan’s passing, then you do the autopsy.” And so, we agreed.
The autopsy revealed Ryan had been living with Hypertrophic Obstructive Cardiomyopathy (HOCM), a relatively new and under-researched condition at that time. This led us to genetic testing, uncovering that my mum, my other brother Darren, and I were carriers of this condition.
My mum is a carrier of the condition with no signs of the condition; my brother Darren is a carrier of the condition, showing signs of a mild case, but has since had a defibrillator fitted in his chest.
I am also a carrier with no signs of having the condition at this point in my life. At 22, amidst grief and trauma, the concept of using IVF along with PGD (pre-implantation genetic diagnosis) to eliminate this gene from our family seemed distant. For context, my mum’s mum passed when she was 35 and her dad when he was 53, so this gene has a long history in our family.
With marriage and the thought of starting a family, the significance of my brother’s legacy became apparent. He sacrificed his life so we could alter our family’s future. Embarking on IVF was a choice, and I was naïve. A choice that I questioned many times throughout the process.
Contrary to the common misconception of IVF as a straightforward procedure, it is more than a mere prescription for pregnancy. Each cycle is a personalised scheduled treatment plan that does not always result in the desired outcome- a pregnancy or baby. I learned this very quickly.
Each IVF cycle came with its wait times, from genetic mapping to multiple cycles resulting in inconclusive or genetically affected embryos. Meaning they either had the HOCM gene or were genetically not suitable for transfer. This meant we did multiple stimulation cycles with no embryos to transfer.
The IVF stimulation cycle itself is an intense regimen of injections, scans, and emotional turbulence. The journey for me was isolating—while friends seemed to conceive effortlessly, I felt alone in my struggle.
Financial strain entered the equation, compelling us to use my superannuation to fund subsequent IVF cycles, but we were in it and were willing to do whatever it took.
Social gatherings became triggers, amplifying the sense of isolation as pregnancy announcements felt like constant reminders of my struggle. Shabbat dinners with family became hard to face.
Being filled with hormones meant I was emotionally explosive,
I was tired,
I was drained,
and my mental health was not ok.
But I kept going because all I wanted was to start a family.
It was a hard, dark time in my life. One that uprooted all the trauma from my brother Ryan’s untimely passing. Grief that I was still processing and continue to process every day.
Finally, after numerous cycles, a glimmer of hope came with one viable embryo. The nerves and excitement in the lead-up to a transfer were intense, only to be met with heartbreak when it did not lead to a successful pregnancy.
I vividly remember being at work when I got the call. I was sure I was pregnant; I had all the symptoms. Bloating, sore boobs, nausea. I had been through the wringer, surely – I have to be pregnant. I took the call with my IVF nurse at work in a little meeting room.
But my excitement was shattered. My very normal day at work turned very quickly – I was not pregnant. My workplace had no idea what I was going through. My work friends had to help me gather my things and I left work and never returned for the remainder of the week. I had no idea what people were thinking but I can only imagine they thought I was unstable.
I spent the next week at home feeling overwhelmed.
Thoughts of:
-How will we be able to afford our next cycle?
-How many more cycles will it take?
-Why is it not working?
Questions no one had the answer to. Support that the clinic did not offer and honestly, I did not want to step foot into a clinic unless it was to pick up medication. I desperately wanted to start a family and we toyed with the idea of just trying naturally. For obvious reasons, we did not.
Through this rollercoaster of disappointment and anxiety, I learned about patience, gratitude, and the enduring power of hope and friendship.
A dear friend undergoing a similar journey became a lifeline, sharing in small victories and providing much-needed understanding and humour in our darkest moments. Even though her journey was different, she felt more inclined to share it with someone going through something similar. We understood one another on a different level. This was my saving grace.
To this very day, this friend has been my ultimate ride-or-die.
Not all friends share their fertility struggles. It is very taboo. I am a little more open with my story because it is my brother Ryan’s legacy.
Eventually, with two embryos, one day-five blastocyst and another inconclusive embryo, came the transfer day filled with nervous anticipation.
Both were frozen. I went in for my transfer. Anxiety filled me that morning.
Would my frozen embryo make the thawing process? Because there is always a risk, it will not. Should we use our inconclusive embryo if we need to? Another risk.
I went for the transfer, an absolute mess. Thank God my beautiful day-five blastocyst thawed.
They put me up on stirrups. Using a guided ultrasound, shot the embryo up into my uterus with a catheter. They always need to leave and return to the lab to check the embryo left the catheter. Mine did not.
I was heartbroken, but my Dr put me back in the chair and assured me, “THIS IS A STICKY ONE” and lo and behold, 14 days later, after a very anxious wait. I was pregnant with my first baby, Taylor.
This was my experience with my first pregnancy, and I will need another hour to share my next.
In closing, I want to highlight the profound gratitude I feel for having had the opportunity to welcome two healthy children into my life through IVF with PGD.
A true testament to how my brother Ryan always looked out for our family. My wish is for anyone navigating a fertility journey—in whatever form it takes — to find the support you require. Sometimes, unexpected support becomes a lifeline in the darkest moments, and I am SO proud of our community for organisations like AJFN.
Thank you.